This is default featured slide 1 title
Go to Blogger edit html and find these sentences.Now replace these sentences with your own descriptions.
This is default featured slide 2 title
Go to Blogger edit html and find these sentences.Now replace these sentences with your own descriptions.
This is default featured slide 3 title
Go to Blogger edit html and find these sentences.Now replace these sentences with your own descriptions.
This is default featured slide 4 title
Go to Blogger edit html and find these sentences.Now replace these sentences with your own descriptions.
This is default featured slide 5 title
Go to Blogger edit html and find these sentences.Now replace these sentences with your own descriptions.
Sunday, May 29, 2011
Myesthenia Gravis Usually Asked Questions
At what age is myasthenia common?
The incidence has two age peaks: one peak in the second and third decades affecting mostly women and a peak in the sixth and seventh decades affecting mostly men.
What groups of muscles are commonly involved?
The muscles affected are as follows, in order of likelihood: extraocular, bulbar, neck, limb girdle, distal limbs and trunk.
What is the differential diagnosis in case of Myesthenia Gravis?
· Botulism.
· Eaton-Lambert syndrome.
Mention a drug that can cause myasthenia.
o-Penicillamine therapy given for rheumatoid arthritis.
What is myasthenic crisis?
Exacerbation of myasthenia. The need for artificial ventilation occurs in about 10% of patients with myasthenia. Those with bulbar and respiratory involvement are prone to respiratory infection. The crisis can be precipitated by respiratory infection and surgery. Such patients should be closely monitored for pulmonary function. Those with artificial ventilation are not given cholinergics as this avoids stimulation of pulmonary secretions and uncertainties about overdosage.
How does a cholinergic crisis manifest?
Excessive salivation, confusion, lacrimation, miosis, pallor and collapse. It is important to avoid edrophonium in such patients.
The incidence has two age peaks: one peak in the second and third decades affecting mostly women and a peak in the sixth and seventh decades affecting mostly men.
What groups of muscles are commonly involved?
The muscles affected are as follows, in order of likelihood: extraocular, bulbar, neck, limb girdle, distal limbs and trunk.
What is the differential diagnosis in case of Myesthenia Gravis?
· Botulism.
· Eaton-Lambert syndrome.
Mention a drug that can cause myasthenia.
o-Penicillamine therapy given for rheumatoid arthritis.
What is myasthenic crisis?
Exacerbation of myasthenia. The need for artificial ventilation occurs in about 10% of patients with myasthenia. Those with bulbar and respiratory involvement are prone to respiratory infection. The crisis can be precipitated by respiratory infection and surgery. Such patients should be closely monitored for pulmonary function. Those with artificial ventilation are not given cholinergics as this avoids stimulation of pulmonary secretions and uncertainties about overdosage.
How does a cholinergic crisis manifest?
Excessive salivation, confusion, lacrimation, miosis, pallor and collapse. It is important to avoid edrophonium in such patients.
Wednesday, May 25, 2011
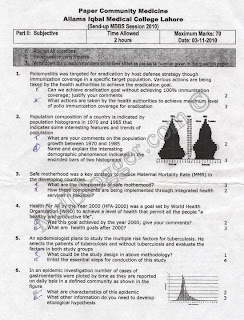
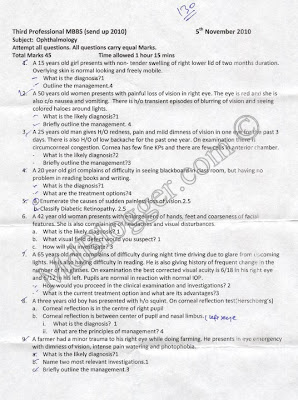
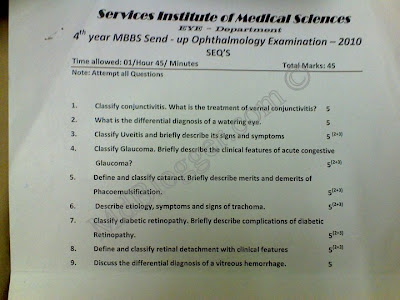
MBBS Fourth Year Ophthalmology (Eye) Sendup Paper 2010
Monday, May 23, 2011
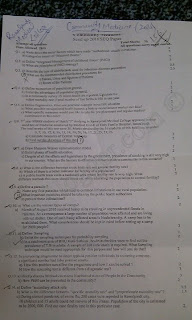
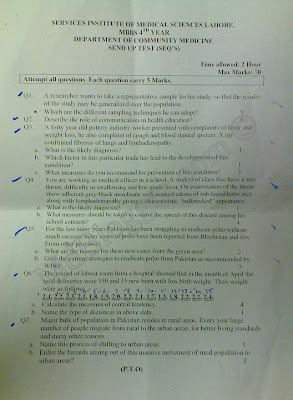
RMC Community Medicine Sendup Paper 2010
Sunday, May 22, 2011
Monday, May 09, 2011
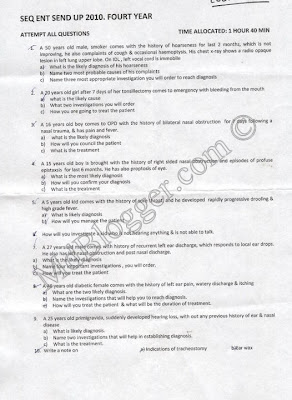
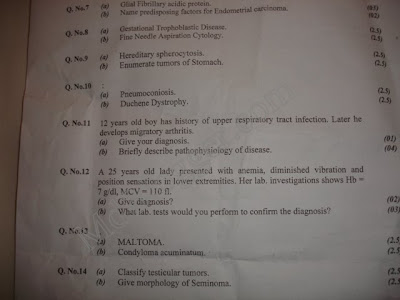
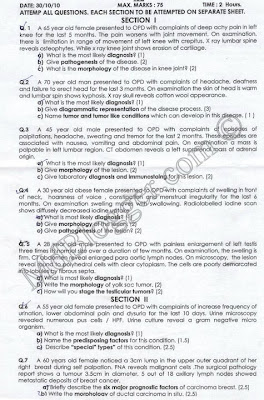
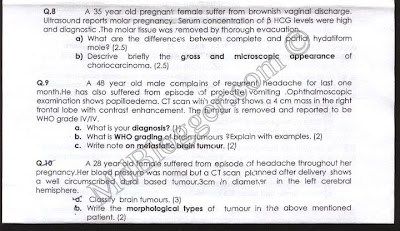
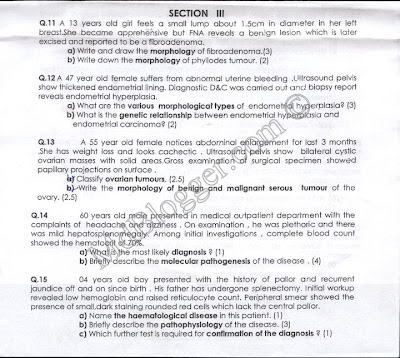
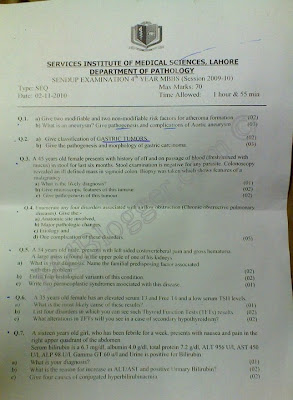
MBBS 4th Year Pathology Sendup Paper 2010
Sunday, May 08, 2011
Community Medicine OSPE 2010 - Part 5
Community Medicine OSPE 9
primary and secondary and tertiary prevention.
Prevention of aids. Secondary attack rate.
age Specific death rate.
Rickets.
Pillars of safe motherhood. Sanitary well.
Dengue.
Polio vaccination schedule
Community Medicine OSPE 10
1 dengue fever(identify vector mode of transmisin)
2 Snake cobra its treatmnt
3 Fruit pic 2 vit its deseases
4 Iceberg disease
5 Shannon weaver model message properties
6 septic tank(2 characteristic nd 2 uses)
7NMR
8GFR
9 oral contacptvz advntge disadvantage
10 measlz vacine dose route complictn
primary and secondary and tertiary prevention.
Prevention of aids. Secondary attack rate.
age Specific death rate.
Rickets.
Pillars of safe motherhood. Sanitary well.
Dengue.
Polio vaccination schedule
Community Medicine OSPE 10
1 dengue fever(identify vector mode of transmisin)
2 Snake cobra its treatmnt
3 Fruit pic 2 vit its deseases
4 Iceberg disease
5 Shannon weaver model message properties
6 septic tank(2 characteristic nd 2 uses)
7NMR
8GFR
9 oral contacptvz advntge disadvantage
10 measlz vacine dose route complictn
How to Perform Rigid Sigmoidoscopy
- Indications:
- Rectal bleeding
- Lower abdominal and pelvic trauma
- Extraction of foreign bodies
- Stool cultures
- Evaluation and biopsy of ileoanal pouch
-
- Contraindications:
- Anal stricture
- Acute perirectal abscess
- Acutely thrombosed hemorrhoids
-
- Anesthesia:None
- Equipment:
- Rigid sigmoidoscope and obturator
- Light source
- Suction apparatus
- Insufflating bulb
- Water-soluble lubricant
- Long cotton-tipped swabs
- Biopsy forceps, if desired
-
- Positioning:Lateral decubitus, lithotomy, or prone jackknife
- Technique:
- Administer tap water or saline enema before procedure to empty distal colon of feces.
- Perform a digital rectal examination to assess for masses.
- Gently insert the sigmoidoscope through the anus to 5 cm, remove the obturator, and attach the light source.
- Judiciously insufflate air to visualize the lumen, using the minimum amount of air necessary to see.
- Slowly advance the sigmoidoscope as a unit to visualize the rectum. Air will leak during the procedure, and intermittent insufflation will be necessary.
- The lumen of the sigmoid will be posterior toward the sacrum and then gently curving to the patient's left. To minimize the risk of perforation, advance the sigmoidoscope only when the lumen is clearly visualized.
- If stool is obstructing the view, use the cotton-tipped swabs to clear the lumen.
- Advance the sigmoidoscope under direct vision as far as tolerated by the patient (most rigid scopes are 20 cm long) (see Figure 5.4).
- To biopsy a mass or polyp, advance the scope until part of the mass is within the barrel of the scope. Insert the biopsy forceps into the barrel, and grasp a specimen of tissue. If needed, silver nitrate sticks may be used to achieve hemostasis.
-
- Systematically inspect the mucosa while withdrawing the instrument slowly.
-
- Complications and Management:
- Bleeding
- Usually self-limited, but may occur after biopsy.
- Rarely will require treatment, but if bleeding is hemodynamically significant, then resuscitate and consider endoscopic treatment.
-
- Perforation
- Manifested by abdominal pain, distention, and loss of hepatic dullness to percussion.
- Obtain upright chest radiograph; free air under the diaphragm confirms the diagnosis.
- IV fluids, IV antibiotics, urgent operative management.
-
-
-
Saturday, May 07, 2011
Community Medicine OSPE 2010 - Part 4
Community Medicine OSPE - 7
1.calculte postnatal
Mortlty rate
2.kawashiokr n wat measurs 2 prevnt it
3.two reasns of somkng.hw wil u educte abt its haZards
4.rabies pre xposure vacine
5.measls n complictn
6.pie chrt n clculte degree
7.cobra bite n its prevnt
8.levls of prevntn
9.diagrm of sludge disposal
Community Medicine OSPE 8
bysinosis ka senario tha wd pic ov coton,
propogtv curv n fctrz afctng spred,
sex ratio n fctrz on wich it dpnds,
polio ki chain ,
cholrmines ki curve ,
tetnaus schedul,
intractv me helth educ abt cancer signs,
ppv n reltv risk calcul,
BMI
Measls vacine ,
iceberg,
nmr,
gfr,
oral pils,
dengue,
weaver shenon model of cmunicatin ,
sand filtrs
1.calculte postnatal
Mortlty rate
2.kawashiokr n wat measurs 2 prevnt it
3.two reasns of somkng.hw wil u educte abt its haZards
4.rabies pre xposure vacine
5.measls n complictn
6.pie chrt n clculte degree
7.cobra bite n its prevnt
8.levls of prevntn
9.diagrm of sludge disposal
Community Medicine OSPE 8
bysinosis ka senario tha wd pic ov coton,
propogtv curv n fctrz afctng spred,
sex ratio n fctrz on wich it dpnds,
polio ki chain ,
cholrmines ki curve ,
tetnaus schedul,
intractv me helth educ abt cancer signs,
ppv n reltv risk calcul,
BMI
Measls vacine ,
iceberg,
nmr,
gfr,
oral pils,
dengue,
weaver shenon model of cmunicatin ,
sand filtrs
Friday, May 06, 2011
Community Medicine OSPE 2010 - Part 3
Community Medicine OSPE -5
SAR and limitatin, safemother hood components and content of clear and safe delivery, health
education about senitary measure to vilage, age specific death rates, ricket and prevent,
hypertensin ke mod factor and 2 bias, denge vector and personal prevent, level of prev and spec
protection for aids, polio vacine and herd imunity.
Community Medicine OSPE -6
1.Cobra bite,management.
2.Strength of sewage
lung cncer ki heatlh eductin,
3.rabies vacintn for pre exposure,
4. kawashkor nd its prventn,
5.PNMR numerical,
6.pie chart wat type of data is it?nd find the degres for 35%
7.primary heatlh cre, dhq facilities
8.popltn pyramid
SAR and limitatin, safemother hood components and content of clear and safe delivery, health
education about senitary measure to vilage, age specific death rates, ricket and prevent,
hypertensin ke mod factor and 2 bias, denge vector and personal prevent, level of prev and spec
protection for aids, polio vacine and herd imunity.
Community Medicine OSPE -6
1.Cobra bite,management.
2.Strength of sewage
lung cncer ki heatlh eductin,
3.rabies vacintn for pre exposure,
4. kawashkor nd its prventn,
5.PNMR numerical,
6.pie chart wat type of data is it?nd find the degres for 35%
7.primary heatlh cre, dhq facilities
8.popltn pyramid
Thursday, May 05, 2011
Community Medicine OSPE 2010 - Part 2
Community Medicine OSPE -3
primary and secondary and tertiary prevention.
Prevention of aids. Secondary attack rate.
age Specific death rate.
Rickets.
Pillars of safe motherhood. Sanitary well.
Dengue.
Polio vaccination schedule.
Community Medicine OSPE -4
Measls vacine ,
iceberg,
nmr,
gfr,
oral pils,
dengue,
weaver shenon model of cmunicatin ,
sand filtrs
primary and secondary and tertiary prevention.
Prevention of aids. Secondary attack rate.
age Specific death rate.
Rickets.
Pillars of safe motherhood. Sanitary well.
Dengue.
Polio vaccination schedule.
Community Medicine OSPE -4
Measls vacine ,
iceberg,
nmr,
gfr,
oral pils,
dengue,
weaver shenon model of cmunicatin ,
sand filtrs
Wednesday, May 04, 2011
Monday, May 02, 2011
How to Perform OroGastric Intubation
- Indications:The indications for orogastric (OG) tubes are generally the same as for NG tubes. However, because they are generally not
- tolerated well by the awake patient, they are used in intubated patients and newborns. The OG tube is the preferred tube for decompressing the stomach in the head trauma patient with a potential basilar skull fracture.
- Acute gastric dilatation
- Gastric outlet obstruction
- Upper gastrointestinal bleeding
- Ileus
- Small bowel obstruction
- Enteral feeding
-
- Contraindications:Recent esophageal or gastric surgery
- Anesthesia:None
- Equipment:
- Levin or Salem sump tube
- Water-soluble lubricant
- Catheter-tip syringe (60 ml)
- Stethoscope
-
- Positioning:Supine
- Technique:
- Measure tube from mouth to earlobe and down to anterior abdomen so that last hole on tube is below the xiphoid process. This marks the distance the tube should be inserted.
- Apply lubricant liberally to tube.
- Because the patients in whom OG tubes are used are generally unable to cooperate, the tube should be placed into the mouth, directed posteriorly, until the tip begins to pass downward into the esophagus.
- Advance the tube slowly and steadily. If any resistance is encountered, stop and withdraw the tube completely. Repeat step c.
- If the tube advances easily, with little resistance, continue until the premeasured distance is reached. Resistance, gagging,
-
- fogging of the tube, or hypoxia suggests errant placement of the tube into the trachea.
- Confirm correct placement into stomach by injecting 20 ml of air with the catheter-tip syringe while auscultating over the epigastric area. Correct placement is also confirmed by aspiration of a large volume of fluid.
- Irrigate tube with 15–20 ml of saline every 4 hours. Salem sump tubes will require injection of 15–20 ml of air through the sump (blue) port every 4 hours to maintain proper functioning.
- Constant low suction may be applied to Salem sump tubes, whereas Levin tubes should have only low intermittent suction.
- Monitor gastric residuals if tube is used for enteral feeding. Obtain a chest radiograph to confirm placement before using for enteral feeding.
- Monitor gastric pH every 4–6 hours and correct with antacids for pH < 4.5.
-
- Complications and Management:
- Pharyngeal discomfort and gagging are a problem with OG tubes when they are placed in awake and alert patients, and essentially eliminates their use in such patients except in conjunction with an oral endotracheal tube.
- Tracheal intubation
- Correct placement in the esophagus is usually evident by the ease of advancement of the tube. Any resistance suggests tracheal intubation or coiling within the posterior pharynx.
- Obtain a chest radiograph to confirm placement prior to use for enteral feeding.
-
- Gastritis
- Usually manifests itself as mild, self-limited upper gastrointestinal bleeding.
- Prophylaxis consists of maintaining gastric pH > 4.5 with antacids via the tube, IV histamine2 receptor blockers, and removal of tube as soon as possible.
-
-
-
-
-