I. Assessing Severity of Burn Injury A. Functions of the Skin:
I. Assessing Severity of Burn Injury A. Functions of the Skin:1. maintains fluid and electrolyte balance
2. protects the body from invasion
3. regulates body temperature
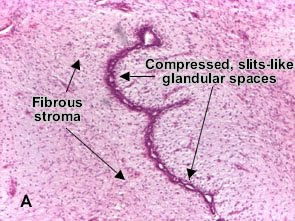
B. Anatomy:1. epidermis
2. dermis (includes epidermal appendages)
3. subcutaneous tissue
4. fascia and muscle
C. Assessment of Burn Depth – related to temperature, time of exposure, and thickness of skin:
1. First degree burn
a. caused by sunburn or flash
b. involves epidermal layer only
c. usually appears red to pink
d. is painful to touch
e. may become slightly edematous
f. heals in 3-5 days (rarely leaves any scar)
g. does NOT count in the burn size calculation
2. Second degree burn (partial-thickness)
a. usually caused by flash, scalds, or brief contact with hot object
b. involves the epidermis and part of the dermis
c. has vesicles and bullae
d. moist appearance – usually red to pale pink
e. tactile and pain sensibility is intact – very painful
f. develops significant edema
g. heals in 7-21+ days with variable amounts of scarring
3. Third degree burn (full-thickness)
a. usually caused by flame, high intensity flash, electricity, chemicals, or prolonged contact with hot liquids or hot objects
b. extends through the epidermis and dermis
c. usually appears white, brown or black; may have thrombosed veins
d. wound appears dry
e. elasticity of the wound is destroyed, so wound becomes leathery and feels firm to the touch
f. marked edema and decreased elasticity may necessitate escharotomies
g. generally painless to touch
4. Escharotomies
a. longitudinal incisions through eschar that release constriction
b. may be necessary in presence of full-thickness circumferential burns of an extremity or chest.
c. assess adequacy of circulation (pulse, capillary refill, movement, numbness, tingling, pain) and elevate
5. Zones of injury
a. zone of coagulation
b. zone of stasis
c. zone of hyperemia
D. Estimation of Burn Size -- calculating per cent Total Body Surface Area burned (%TBSA):
1. Rule of Nines
Adults Infants
head and neck 9% 18%
each upper extremity 9% 9%
anterior trunk 18% 18%
posterior trunk 18% 18%
each lower extremity 18% 14%
perineum 1% 1%
100% 100%
2. Lund and Browder Chart (see attached)
3. Rule of the Palm
a. the patient’s anterior hand is approximately 1% of his body surface area
b. useful in estimating burn size of splash-injuries or small burns
E. Burns of Special Areas:
1. face, ears
2. hands
3. feet
4. joints
5. perineum
II. Care of Some Special Types of Injuries:
A. Tar, wax
B. Chemical injuries
1. pathophysiology
2. treatment
3. chemical burns to the eyes
C. Electrical injuries
1. pathophysiology
2. problems associated with electrical injuries
a. types of wounds
- contact points (entry and exit)
- arc wounds
- flame burns
b. cardiac
c. pulmonary
d. gastrointestinal
e. renal
f. neurologic
g. musculoskeletal
3. sequelae of electrical injuries
D. Burns associated with Child Abuse
1. history requiring closer evaluation
2. appearance of suspicious burns
3. documentation required
III. Smoke Inhalation:A. Carbon Monoxide poisoning (kills during and immediately following the fire)
1. CO from the fire combines with the circulating hemoglobin, bumping the oxygen from its receptor sites
2. signs of CO poisoning include confusion, dizziness, headache, nausea
3. treatment: administration of 100% oxygen
B. Upper airway obstruction
1. burns of the face, mouth, tongue, pharynx results in massive edema formation and the potential for airway obstruction
2. edema continues to develop for up to about 24 hours
3. treatment: intubate to mechanically maintain airway patency
4. edema will usually decrease at about post-burn day #3, and the patient may then be able to be extubated
C. Pulmonary injury from the chemicals inhaled
1. patient develops ARDS over the first 24 hours post-injury
2. pneumonia may also occur (sometimes as late as 10 days post-burn)
IV. Fluid Resuscitation:
A. Pathophysiology of “Burn Shock”
1. fluid shifts
2. decreased cardiac output
3. electrolyte and hematologic alterations
4. renal effects
5. central nervous system effects
6. compensation for “burn shock”
a. effects on skin
b. effects on gut
B. Fluid Resuscitation (in the first 24 hours post-burn)
1. Baxter (or Parkland) formula:
(4ml of Ringers Lactate) x (% burn) x (kg weight) = mls required in first 24 hrs
½ is given in the first 8 hours (calculated from time patient was burned)
¼ is given in the second 8 hours
¼ is given in the third 8 hours
EXAMPLE: 4 ml / 70 kg / 50% TBSA = 14,000 ml fluid resuscitation required
(7 liters given in first 8 hours)
2. IV access guidelines:
a. <> 45% TBSA: secure 2 large bore IV lines in upper extremities
3. Pediatrics (children 0-3 years) – add maintenance fluids as D5¼ NS to Baxter formula
4. Evaluation of adequacy of fluid resuscitation
a. alert sensorium
b. adequate urine output (>30 ml/hr in adult; 1 ml/kg/hr in children up to 30 kg)
c. slightly high normal pulse, usually about 100
d. normal blood pressure for age
e. relief of paralytic ileus or nausea
V. Initial Treatment:
A. History for initial assessment
1. type of burn
2. history of flame burns / closed-space accident?
3. circumstances surrounding the injury (LOC, seizure, fall, crash, blast)
4. pre-existing diseases and medications
5. first aid measures already taken
B. Emergent Care
1. maintain an adequate airway and begin oxygen
2. assess for associated life-threatening injuries
3. initiate fluid therapy
4. insert foley catheter to monitor hourly urine output (burns >25% TBSA)
5. insert nasogastric tube (burns > 20% if air transport is planned)
6. keep patient warm (!)
7. elevate burned extremities; monitor pulses
8. tetanus prophylaxis
9. pain management (small IV doses only)
10. psychological support of patient and family
C. Advanced Burn Life Support Burn Center Referral Criteria:
1. full-thickness (3rd degree) burns
2. partial-thickness (2nd degree) burns >10% TBSA
3. burns of special areas
a. face, hands, feet, genitalia, or across major joints
b. circumferential full-thickness burns of an extremity or trunk
4. electrical injuries
5. chemical injuries
6. patients with inhalation injury in addition to burns
7. patients with pre-existing disease
8. patients with concomitant trauma
Transport
Wrap patient in dry sheet and blanket for transfer (sterile if you have it; clean if you don’t)
No ice or (cold) soaks
Don’t apply topical antibiotics before transport, unless transfer is delayed.
VI. Wound Care:
A. Initial wound care
1. isolation: scrubs or gown, mask, gloves
2. cleanse wounds; blisters are usually debrided if patient will be admitted
3. shave as needed; never shave eyebrows
4. topical agents as ordered (not usually necessary at referring hospital)
B. Daily wound care
1. pain medication is needed prior to dressing changes
2. dressings may usually be soaked off
3. remove any old cream and gently wash wounds
4. debride any loose tissue
5. reapply topicals and dressings as ordered
C. Assess daily for signs of infection
1. cellulitis (redness, heat, swelling)
2. darkening of the eschar
3. odor
4. purulence or greenish drainage
5. deterioration of a healing wound
D. Assess for early signs of sepsis
1. disorientation
2. decreased urine output
3. metabolic acidosis
4. tachypnea
5. tachycardia
6. paralytic ileus or vomiting
7. hyperglycemia
8. hyper- or hypo-thermia
E. Debridement
1. if you can get between dead and viable tissue, the dead tissue should be removed
2. mechanical debridement by nurses should not cause bleeding
3. some debris will come off with coarse mesh gauze dressing changes
4. most patients are not debrided under general anesthesia in the OR
a. tangential excision – shave layer by layer until a bleeding (viable) bed is produced (to maximize tissue salvage)
b. primary or fascial excision – separate tissue at fascial layer to minimize blood loss
F. Topical Antibiotics
1. Silver sulfadiazine (Silvadene, Flamazine, Thermazine, SSD)
a. a water-soluble cream which is locally non-toxic
b. bactericidal spectrum against a wide range of gram+ and gram- organisms and candida albicans
c. pain-free application
d. softens the eschar; may combine with exudate to form a gelatinous layer
e. few side effects: is generally applied once daily
2. Mafenide acetate (Sulfamylon)
a. a water soluble cream or, or a powder that may be mixed with saline
b. bacterial spectrum: gram+, gram – organisms, some anaerobes, but not yeast
c. hypersensitivity reactions (rashes) to sulfa are sometimes seen
3. Bacitracin and other petroleum ointments
a. “benign” topicals which mostly contain moisture
b. microbes may become resistant
c. typically used for scrapes and abrasions
4. Muperacin (Bactroban)
a. an ointment used against gram+ organisms
b. used when methacillin resistant staph aureus (MRSA) is found in wounds
c. should also be applied to nares, when used
5. Silver Nitrate (bulky wet dressings)
a. AgNO3 isn’t used much anymore because it stains everything black
b. A 0.5% solution of AgNO3 in water – keep dressings wet so that concentration of AgNO3 doesn’t increase (concentrated AgNO3 is caustic to wounds)
c. water-soaked dressings are uncomfortable and can leech electrolytes
6. Acticoat
a. a slow-release silver-impregnated dressing
b. silver is released by water (either from the wound or exogenously applied) for about 3 days
c. is being used on shallow wounds and donor sites to decrease dressing changes
G. Grafting
1. Xenograft or Heterograft (used as a biologic dressing)
a. animal skin (usually pig) which is used as a temporary wound coverage
b. is applied to a clean shallow wound, to protect it until it heals
c. dries and separates from the wound, as the wound heals underneath
2. Allograft or Homograft (used as a biologic dressing)
a. non-self human skin (usually cadaver) which is used as temporary wound cover
b. if left in place long enough (> 5 days) it will become vascularized, and will have to be excised in OR to remove it
c. if left in place long enough, patient may develop a rejection reaction to it
d. used to “buy time” and temporarily close a wound until patient’s own skin is available
e. used as a “test graft” to determine if a wound is ready to accept a skin graft
3. Autograft
a. skin taken from one area of the patient’s body to another
b. sheet graft
- whole graft is laid intact on wound
- used in cosmetic areas of the body (face, neck, hands)
- require meticulous care post-op to prevent fluid accumulation beneath it
c. meshed graft
- passed through a machine that creates slits in it – so it can be expanded
- is often wrapped, with no dressing changes, for first 3-5 days after application
d. donor site – area that gives up skin used in skin graft
- is often more painful than burn wounds
- may be covered with a dressing or topical; heals by epithelialization
4. Integra
a. is placed on a newly excised wound (after all dead tissue is removed)
b. becomes vascularized, forming a “neodermis” over about 3 weeks
c. is grafted with thin epidermal grafts after the new dermis develops
VII. Rehabilitation:
A. Beings at the time of admission
B. Prevention of contractures
1. exercising
2. positioning
3. splinting to maintain stretch
C. Minimizing scarring
1. elasticized circular bandage initially
2. custom fitted pressure garments
3. may require silicone inserts
D. The nature of scars
1. can’t easily predict who will scar, but partial thickness wounds that heal over more than 3 weeks tend to scar the most
2. scars will become redder and firmer 6-8 weeks after the wound heals; then will begin to blanche out and soften over about a 1-year period
3. Scars may tingle, itch or burn as they mature
E. Other post-hospitalization issues
1. body-image changes
2. role changes
3. uncomfortable sensations in burns
4. changes in sweating pattern
5. fatigue
6. return to work / school
7. PTSD
F. Interventions
1. motivational strategies
2. reconstructive surgery
3. tissue expanders
4. make-up consultation
5. tattooing (for color match)
6. support groups